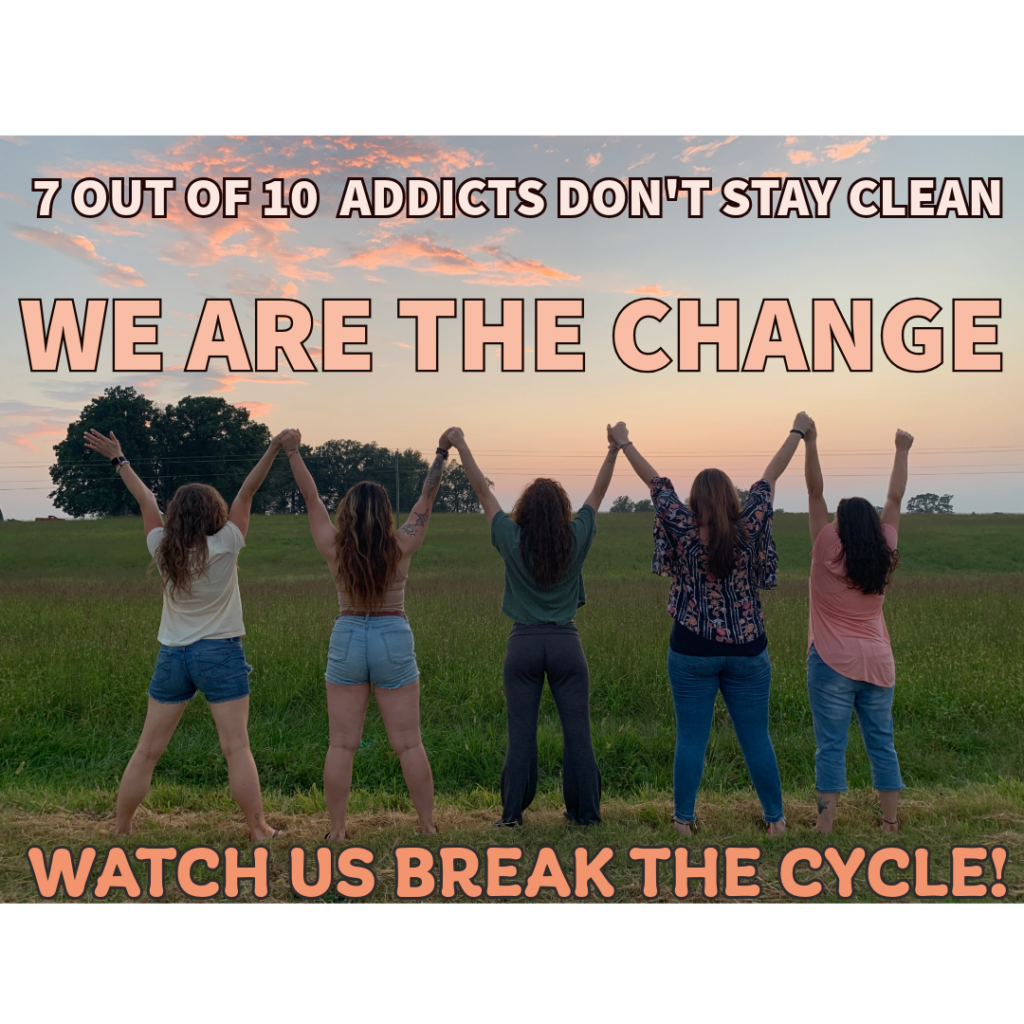
A commitment to a better world
Women’s Extended Care Center Substance Use Solution

A passion for saving lives
Recovering Hands is dedicated to providing support and residential extended-care to women suffering the effects of substance abuse. Through working with a consistent advising team of peer recovery support specialists familiar with each resident, and with input from the community, residents learn to recognize and manage the symptoms of illness and the hallmarks of addiction, acquiring the tools to reduce the impact of these devastating forces on their lives.
Peer Support
“Through shared understanding, respect, and mutual empowerment, peer support workers help people become and stay engaged in the recovery process and reduce the likelihood of relapse. Peer support services can effectively extend the reach of treatment beyond the clinical setting into the everyday environment of those seeking a successful, sustained recovery process.” (SAMHSA)
Residential Support
To provide quality substance abuse residential support services leading to improved health, wellness, long-term recovery, employability and reintegration with society and families.
Life Skills
Life skills workshops geared towards learning how to shop and prepare nutritional meals, improved time management skills – balancing life, children, work, recovery, how to buy and maintain a vehicle or take public transportation, budgeting 101, how to create a resume, seeking gainful employment, becoming a useful productive member of society.
Onsite Gym
Creative and individualized application of recovery oriented life skills, exercise classes, access to our on site gym, yoga and meditation.
Equine Assisted Healing
Included are opportunities to work with horses and other animals on the farm to develop better self-care, greater self awareness and interpersonal skills.
And So Much More
Farming, ranching, wood working, gardening, canning, candle making, pottery, and soap making
What we do and who we are
Please Donate Today!
- Scholarships
- Building Fund
- Tax Deductible Donations
- Thank you for considering making your tax deductible donation to Recovering Hands today.

Recovering Hands Newsletter
- Stay up to date with Recovering Hands Events
- Read what’s new
- See us “in the news”
“Recovering Hands did more for me in those few short months than anyone could ever know.“
Amanda M
Virginia Beach, VA
Watch, Read, Listen
Join our subscribers
Stay in the loop with everything you need to know.
